About Altitude Sickness
By 37 BC, the ancient Chinese documented an unusual and strange illness when they trudged the passes of what they later called the Little Headache and Great Headache mountains. They named these mountains for the splitting headaches and vomiting they inflicted on passing travelers and their donkeys.
Jesuit priest, Jose de Acosta, was the first westerner to define mountain sickness, who accompanied the Spanish Conquistadors in Peru. Thereafter, researchers have described the consequences of travel to high altitudes and named the syndrome acute mountain sickness (AMS). Generally, acute mountain sickness occurs if you walk or climb too rapidly to a higher elevation.
Travel to the altitude above 2,500 m is related to the risk of developing 1 or more forms of acute altitude illness: acute mountain sickness (AMS), high altitude cerebral edema (HACE), and high altitude pulmonary edema (HAPE).
The Wilderness Medical Society (WMS) has recently published a 2019 update on its guidelines for the prevention and treatment of acute altitude illness. The WMS guidelines, collected by a team of ten experts from across the country and published in Wilderness & Environmental Medicine.
The guidelines address the acute altitude illness, which can strike to the person who travels rapidly to an altitude that he/she is not familiar with or used to with, as contrasting to the chronic mountain sickness that can affect people who reside permanently at high elevations.
Particularly, the risks of high altitude arise when ascending beyond 2,500m /8,200 ft. People who suffer from severe lung, heart, and blood diseases are prone to develop AMS. Even, healthy young adults who take part in energetic activity upon arrival at elevation are also likely to suffer from AMS
The “susceptible individuals” can develop AMS and possibly HAPE at altitude as low as 2,000m/ 6,500 ft. Individuals with a previous history of high altitude sickness and who have been living at low elevation prior to climb are mainly susceptible. Diagnoses of AMS, HAPE, or HACE should not be let off based on the fact that a susceptible individual is below 2500 m.
The early symptoms of AMS is followed by mild headache, fatigue, nausea, dizziness, which are pretty non-specific. Therefore, it’s significant to think through other possible reasons like severe dehydration and hypernatremia, pneumonia, carbon monoxide poisoning, and hypoglycemia.
Therefore the preventive procedures should be considered depending on the elevation to which the individual is traveling and also considered for the other aspects like a history of performance at high altitude, rate of ascent, and availability of rest days.
Generally, there are three types of acute altitude sickness which are detailed as follows:
Acute mountain sickness and high altitude cerebral edema (HACE)
Acute mountain sickness is the mildest form and very common sickness that happens when a person who is used to being at a low elevation ascends to a higher altitude. The symptoms of AMS include headaches plus there is one or more of the following symptoms: fatigue, poor appetite, nausea or vomiting, light-headedness, and sleep disturbances.
The Lake Louise consensus group described acute mountain sickness as the occurrence of headache in the non-acclimatized individual who has lately arrived at an altitude above 2500 m and the presence of one or more of the following symptoms:
- Gastrointestinal symptoms like anorexia, nausea or vomiting, b) insomnia, (more than the just usual waking) c) dizziness d) tiredness or fatigue
Typically, symptoms develop within 6 to 12 hours after ascent but occasionally as early as 1 hour and can range from mild to severe. Symptoms usually improve after 1 to 2 days unless one has moved to a higher altitude but they can sometimes last longer.
In AMS, the sufferer’s level of consciousness is normal. The Lake Louise Score can be useful as a guide to measure your diagnosis of AMS and assess progression.
In less than 1% of cases, symptoms can progress to high-altitude cerebral edema, (HACE), in which the brain becomes dangerously swollen with fluids.
HACE is the most severe form of altitude sickness which takes place when three is an accumulation of fluid in and around the brain. It is a life-threatening state marked by severe headache, confusion, lethargy, lack of coordination, irritability, vomiting, seizures, coma, and eventually death if untreated. A person with HACE may look like a confused, disoriented drunk person, fumbling with clothing, unable to walk a straight line, and with slurred speech.
From a clinical perspective, HACE denotes a very severe form of AMS; so, preventive and treatment procedures for the 2 disorders can be addressed simultaneously
The distinct between AMS and HACE is that AMS generates a number of symptoms which, in medical terminology, are feelings reported by a patient. HACE also produces signs which are indicators that can be detected and noticed independently by a doctor. For instance, Feeling dizzy is a sign of AMS, but if the dizziness is so worst that then the patient has to undergo through the type of balance test to get in a sobriety check, that indicates ataxia (a neurological sign comprising of absence of voluntary coordination of muscle movements that can include gait abnormality, speech changes, and abnormalities in eye movements.), a possible sign of HACE brain collects extra fluid, swells and stops working properly.
Prevention from AMS and HACE
Rate of Ascent and Acclimatization
The foremost emphasize and reasonable approach to avoid all sorts of altitude sickness is to ascent slowly. Even before you reach to possibly precarious altitude, it may aid to spend a night at an intermediate altitude. WMS guidelines recommend that while you climb beyond 3,000 meters/ 10,000 feet, you should not exceed your sleeping altitude by more than 500 meters each day.
In addition, an extra rest day must include once every three to four days. On acclimatization day, do not over-exert yourself. However, If the landscapes and other logistics issues influence you to ascend beyond 500 meters per day then, plan an additional day for acclimatization to keep the average ascent below 1,500 ft./day over the whole trip. (i.e. The total altitude gain divided by the number of ascent throughout the trip) For those at low risk, prevention is primarily a gradual ascent without medication
Preventive treatment with medicine
The rates of acclimatization and physiologic responses to high differ significantly between individuals. The approach to the prevention of AMS and HACE should be a function of the risk profile of the individual traveling to high elevation.
Medicine is the next best alternative to prevent altitude illness which can be used depending on the risk profile of both the trekker and the trip. It is easy to predict your future susceptibility if you had altitude illness previously. Whereas, if you have a prior history of high altitude illness then you might want to consider preventive drugs that might help you if you are trekking in an inaccessible and secluded area.
|
Risk categories for acute mountain sickness |
|
|
Risk category |
Description |
|
Low |
• Individuals with no history of altitude illness and ascending to ≤2800 m |
|
• Individuals taking ≥2 d to arrive at 2500–3000 m with subsequent increases in sleeping elevation <500 m·d−1and an extra day for acclimatization every 1000 m |
|
|
Moderate |
• Individuals with history of AMS and ascending to 2500–2800 m in 1 d |
|
• No history of AMS and ascending to >2800 m in 1 d |
|
|
• All individuals ascending >500 m·d−1 (increase in sleeping elevation) at altitudes above 3000 m but with an extra day for acclimatization every 1000 m |
|
|
High |
• Individuals with a history of AMS and ascending to >2800 m in 1 d |
|
• All individuals with a history of HACE or HAPE |
|
|
• All individuals ascending to >3500 m in 1 d |
|
|
• All individuals ascending >500 m·d−1 (increase in sleeping elevation) above >3000 m without extra days for acclimatization |
|
|
• Very rapid ascents (eg, <7 d ascents of Mt. Kilimanjaro) |
|
Extracted from Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of Acute Altitude Illness: 2019 Update
According to WMS, the preferred choice of preventative drug is acetazolamide (Diamox), to treat both AMS and HACE. This drug should be taken beforehand you initiate ascending and keep on having till two days after you reach your highest elevation or you start descending, whichever comes first.
The usual adult dose is 125 mg which should intake every 12 hours. For those intolerant or allergic to acetazolamide, dexamethasone may be used. In special, emergent situations necessitating rapid elevation gain, both drugs may be used simultaneously. For example Military or rescue teams that must ascend speedily beyond 3,500 meters without acclimatization.
Acetaminophen and Ibuprofen can be used to treat and relieve headache at high elevation but has not been found to improve the full spectrum of AMS symptoms or effectively treat HACE
Descent
The best way to prevent AMS and HACE is decent to lower altitude ranging from 1000 to 3000 feet but the required decrease in altitude differs among individuals. Individuals should head down till warning sign resolve if terrain, weather, or injuries make descent impossible.
Lake Louise Questionnaire
AMS, HACE, and HAPE can be assessed daily using the Lake Louise Consensus symptom score. It is a questionnaire-based indicative tool that can be applied to diagnose acute mountain sickness. This system is the most general technique to check how bad your altitude illness symptoms are. A score between three and six is an indication of mild to moderate altitude illness, scores over six-show severe altitude sickness.
Supplemental Oxygen
If you’ve got HACE, there are some more complex countermeasures like supplemental oxygen and portable hyperbaric chambers.
Supplemental oxygen provides an appropriate alternative to descent. The Oxygen supplied by nasal cannula or mask at flow rates adequate help to get rid of symptoms
A peripheral capillary oxygen saturation (SpO2) >90% is generally adequate. Usually, the oxygen used in the condition when the descent is recommended but not possible (e.g. dangerous terrain or weather, not enough helpers to carry an unconscious victim, waiting for a helicopter) or to relieve severely ill individuals during descent.
Portable hyperbaric chambers
When descent is not feasible, and supplemental oxygen is unavailable then portable hyperbaric chambers should be used for a victim with severe AMS or HACE.
Once the individual is taken out from the chamber, the symptoms may still remain however this should not stop the use of the chamber when indicated
In many circumstances, ill individuals may recover sufficiently to allow them to assist in their evacuation and descend after symptoms improve.
The suggested Treatment approach to AMS/ HACE
One should take careful attention to prevent disorders whose symptoms and signs were similar to those that appear with AMS and HACE, for example, carbon monoxide poisoning, dehydration, exhaustion, hypoglycemia, hypothermia, and hyponatremia. Persons with AMS of any severity or HACE should stop ascending and may require heading down depending on the nature of illness and the conditions.
Patients with AMS can stay at their existing elevation and can take acetaminophen (Tylenol) or ibuprofen for the headache, and an antiemetic like Gravol for nausea and vomiting.
These individuals should be thoroughly and carefully observed for signs of progression of altitude sickness.
If the symptoms deteriorate or didn’t see any improvement after 1 or 2 days then the victim should move to a lower altitude.
|
Acute mountain sickness classification |
|||
|
Category |
Mild AMS |
Moderate–Severe AMS |
High altitude cerebral edema (HACE) |
|
Symptoms |
Headache plus 1 or more other symptoms (nausea/vomiting, fatigue, lassitude, dizziness) |
Headache plus 1 or more other symptoms (nausea/vomiting, fatigue, lassitude, dizziness) |
Worsening of symptoms seen in moderate to severe AMS |
|
All symptoms of mild intensity |
All symptoms of moderate-severe intensity |
||
|
Signs |
None |
None |
Ataxia, severe lassitude, altered mental status, encephalopathy |
|
Lake Louise AMS Score |
3–5 |
6–12 |
Not applicable |
Extracted from Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of Acute Altitude Illness: 2019 Update
High-altitude pulmonary edema (HAPE)
High-altitude pulmonary edema (HAPE), is completely different from AMS and HACE. HAPE is mainly a pulmonary disorder, whereas acute mountain sickness (AMS) and the much less frequent high-altitude cerebral edema (HACE), are neurologic disorders.
It is a life-threatening emergency in which vessels in the lungs compress causing increased pressure. This causes fluid to leak from the blood vessels to the lung tissues and eventually into the air sacs. When this occurs, the person will be more breathless, which in turn deteriorates the condition from the build-up fluid in the lungs.
HAPE may develop very rapidly (in 1 to 2 hours) or very gradually over days. It often develops during or after the second night at a new altitude. HAPE leads to dyspnea (shortness of breath), reduced physical performance (tiredness, fatigue), tachycardia (rapid heart rate), and the lips may go blue and body temperature may rise and decreased arterial oxygen levels. HAPE varies in degree from very mild to potentially fatal. If it is not treated on time then the condition of the victim progress to unconsciousness, coma, and death.
Mostly, this symptom occurs in a non-acclimatized person who rapidly ascent to an elevation greater than 2,500-3,000 meters and has remained in that environment.
SUGGESTED APPROACH TO HAPE PREVENTION
Gradual ascent is the main recommended method for preventing HAPE. If you trek at high elevation, acclimate yourself slowly. At elevations above 3000 m (approximately 8,200 ft), sleeping altitudes should be limited to an ascent rate of 500 m. An extra acclimatization day with rest should be added.
Nifedipine aids to reduce chest tightness and ease breathing. Pharmacologic prophylaxis is recommended as an adjunctive treatment for individuals with a previous history of HAPE, particularly multiple episodes. In such case, Nifedipine is the preferred drug; it should be taken the day before ascent and keep on having either until descent is started or if the individual has stayed 4 days at the highest elevation, possibly up to 7 days if the individual’s speed of ascent was quicker than suggested
The recommended dose is 30 mg of the extended-release preparation administered every 12 h.
It should be noted that periods are longer than the use of acetazolamide for AMS prevention. For individuals rising to a high point and then heading down toward the trailhead, prophylactic (preventive) drugs should be ceased when the descent is started.
Likewise, an additional examination is required before tadalafil or dexamethasone can be recommended over nifedipine for prevention. Tadalafil can be used for HAPE prevention in identified susceptible individuals who are not candidates for nifedipine. Likewise, Dexamethasone can be used for HAPE prevention in known susceptible individuals who are not candidates for nifedipine and tadalafil.
Acetazolamide medicine can be taken for the prevention of reentry HAPE in people with a history of the disorder. In general, this drug helps acclimatization but should not be depended upon as the sole prophylactic mediator in known HAPE-susceptible individuals.
Treatment of HAPE
The most consistent and best treatment for HAPE is immediate descent, supplemental oxygen and rest while remaining at high altitude are sufficient treatment for mild to moderate HAPE
Before starting treatment, consideration should be given to other reasons for respiratory symptoms at high elevation, such as asthma, bronchospasm, mucous plugging, pneumonia, pneumothorax, pulmonary embolism, viral upper respiratory tract infection, or myocardial infarction.
If HAPE is suspected or diagnosed, oxygen should be started if obtainable, and the patient should be headed down to lower altitudes.
If descent is not possible (harsh weather, delayed helicopter evacuation), then supplemental oxygen should be continued or the individual should be kept in a portable hyperbaric chamber.
Patients who have access to supplemental oxygen and can be effectively supervised and observed in a medical setting may not require to descend to a lower altitude and can be cured with oxygen only at the existing altitude.
In more remote settings, early descent should be considered. if oxygenation cannot improve with supplemental oxygen, if the patient’s condition worsens even with achieving an oxygen saturation >90%, or if the patient didn’t show the sign of progress with proper interventions for HAPE.
In the scenario or circumstances, where resources are inadequate, nifedipine can be used as an aide to descent.
It should only be used as key therapy if none of these other measures (supplemental oxygen, or portable hyperbaric therapy) is available.
A phosphodiesterase inhibitor may be used if nifedipine is unavailable, but concurrent use of multiple pulmonary vasodilators is not recommended.
Likewise, Continuous positive airway pressure (CPAP) can be taken as an assistant to supplemental oxygen and nifedipine can be added if the patient fails to react to oxygen therapy alone.
In the treatment of HAPE, there is no proven role for beta-agonists, diuretics, acetazolamide, or dexamethasone
However, dexamethasone should be considered when a concern is raised for existing HACE.
Individuals who develop HAPE may consider further ascent to higher altitude or re-ascent only when symptoms of HAPE have completely resolved and they maintain stable oxygenation at rest and with mild exercise while off supplemental oxygen and/or vasodilator therapy.
Consideration may be given to using nifedipine or another pulmonary vasodilator upon resuming ascent.
DO CHILDREN GET AMS?
Children develop a similar sort of symptoms of altitude illness as adults and have the same occurrence of AMS. Children are unlikely to suffer from acute mountain sickness or HAPE than are adults. Nevertheless, young kids cannot express or talk about their symptoms well and there is some concern altitude illness may be under-diagnosed in this group. AMS in young children may happen as any of the following symptoms:
- Fussiness and irritability
- Increased crying
- Refuse to eat food
- Lack of energy, or increased drowsiness
- Nausea
- Tiredness/ fatigue
The same principle of prevention in adults apply to children:
- Gradual ascent, and spending a night at a moderate altitude considerably reduce your child’s chance of AMS.
- Ibuprofen or Tylenol will avoid the headache
- Children may also take Diamox to get rid of AMS. Special pediatric dosing of 3-5mg/kg per day applies for children.
- Mild symptoms can be cured with rest, Tylenol or ibuprofen. Children that seem ill should be taken to a physician for medical care. Treatment is similar to adults and comprises oxygen, Diamox, dexamethasone, or mediations for nausea and vomiting.
- HAPE can develop on a child, just as adults do., Children who reside at high elevation seem to get return HAPE more easily than adults.
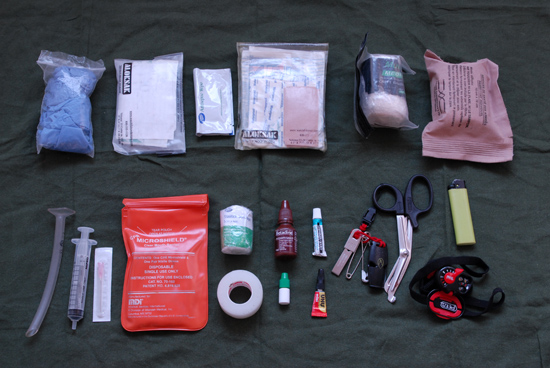
Nepal Sanctuary Treks furnished with indispensable medical supplies like comprehensive first aid kit, trained guides, and Portable Chamber. Our itineraries contemplate many gradual ascents, depending on the duration of the trek. We design the itineraries considering the rest days and altitudes that suit family, solo and school groups.